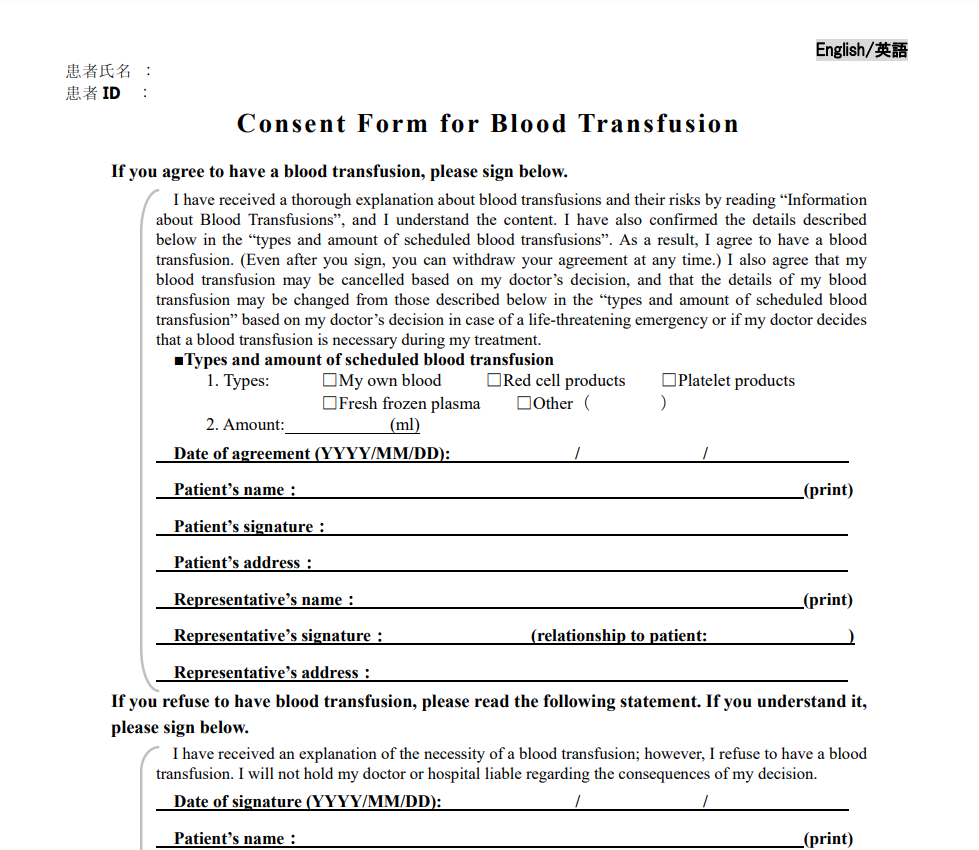
Consent Form Blood Transfusion – On the first page of a consent to transfusion form on which the patient is asked to answer questions about whether they feel at ease with a particular type or blood-related product. This form can be a valuable information source. However, it will also confirm the decision made on the first page. Another page can be used to keep track of the patient’s preferences and to ensure it is that blood transfusion procedure is done in a proper manner. After the patient is aware of the reason for the transfusion, is able to fill out the form.
Questions posed on the consent form
Consent to blood transfusions in a manner that is informed is required for every patient who receives treatment, which includes optional blood transfusions. It is essential to ensure that the person receiving transfusion is competent and uninvolved and has all the knowledge required to understand the procedure. While consent can be granted in writing but written consent is preferred to ensure legality. The consent form should contain the details about the treatment in plain language as well as the anticipated benefits and any negative consequences that could result from the procedure.
An original copy of the completed consent form is required to be kept in the patient’s file at the bedside. In the event that the patient signed permission for continuous transfusion support the consent form should specify the date of expiration. This consent form should contain the “For your information” flag for EMR patients. The flag is in effect until the patient decides to change their decision. Once the consent form must be reviewed to ensure any future transfusions. Make sure that the patient is given the informed consent form prior to when he is a victim of a major bleeding event.
When most patients said that they were provided with the chance for questions to be asked during transfusion, some residents said that just 41percent of the patients actually took their time asking questions. Patients who were given the chance to ask questions, however, did not discuss the time limitations related to the procedure. In the end, the lack of communication between the patients and residents might hinder a patient from asking questions, and patients might be reluctant to ask questions. This could have led to an insufficient understanding among patients about the process and its advantages.
Time of consent meeting
While the advantages of a blood transfusion are considerable however, the risks are just as significant. Patients who receive a transfusion must be fully informed of the risks and benefits as well as the right to refuse. We’ll discuss the importance of obtaining consent, as well as the available resources to assure that people are well-informed and comfortable about the procedure. In the end, you can avoid mistakes in medicine by ensuring that the transfusion experts are aware of the risks associated with blood transfusion.
A single consent can be used to authorize one or more transfusions in hospitalization or during the course of treatment for a patient. The treatment course can be defined by the duration from diagnosis to resolution of the issue. A single consent, thus is valid for all transfusions that are given in hospital settings and also those that are given to outpatients. Since patients could require multiple blood transfusions throughout their life, it’s crucial to have permission for each one from the beginning.
The study examines the process of using a transfusion consent practice in Oman. The results showed that compliance was very high among specialists in haematology however, not in all departments. Another common mistake was the lack of witness’s names. For children two-thirds of consent forms were missing the name of the doctor, whereas 95% contained the name of a parent or guardian and signature.
The patient’s understanding of the reason behind transfusion
If a patient is aware of the necessity of blood transfusions is crucial to an effective outcome. Although separate informed consent is required in certain countries, it does not guarantee that patients are aware of the benefits and risks. Furthermore there are patients who may hesitate to give consent because of religious or cultural motives. This confusion should be corrected before transfusions are able to be administered. This study examines the consent procedure and information given to patients. The study also examines the patient’s understanding of the discussions and the perception of their knowledge about transfusion. Three hundred and forty-two adults took part as part of the investigation.
To determine if the patient will be willing to accept an organ transplant, doctors employ different methods. It is based on the doctor’s expertise and education and also the traditional medical norms. In many cases the patient won’t receive all blood. Instead the blood of a single donor is divided into platelets and red blood cells and then taken to a laboratory for analysis. The result is that the blood will be safe to four patients and not a risk in the case of the patient.
Doctors who have an experience in family medicine, internal medicine medical, or surgery were significantly more successful than residents. Similar is the case for surgeons. The scores for these two groups were similar. Internal medicine and senior physicians doctors scored slightly better than residents. Furthermore, doctors who have an knowledge of the field in blood management that is restrictive were more successful on this test. What is the people’s understanding of the rationale for transfusions vary?
Download Consent Form Blood Transfusion 2024